

临床荟萃 ›› 2024, Vol. 39 ›› Issue (2): 101-107.doi: 10.3969/j.issn.1004-583X.2024.02.001
• 循证研究 • 下一篇
收稿日期:2023-06-12
出版日期:2024-02-20
发布日期:2024-04-18
通讯作者:
游川
E-mail:2164@nsmc.edu.cn
基金资助:
Gong Caifang1, Zhao Junyu1, You Chuan2( )
)
Received:2023-06-12
Online:2024-02-20
Published:2024-04-18
Contact:
You Chuan
E-mail:2164@nsmc.edu.cn
摘要:
目的 系统评价接纳与承诺疗法(acceptance and commitment therapy,ACT)对癌症患者心理健康和生活质量的影响。方法 检索建库至2022年11月在CBM、万方、知网、维普、PubMed、Cochrane Library、Web of Science、EMbase数据库发表的有关ACT对癌症患者心理健康和生活质量影响的随机对照试验。由2名研究者根据纳入及排除标准独立筛选文献、质量评价并提取数据,采用RevMan 5.4进行meta分析。结果 共纳入14篇文献,1 063例癌症患者。Meta分析结果显示,ACT在改善癌症患者的焦虑[SMD=-1.04,95%CI (-1.19,-0.89),P<0.01]、抑郁情绪[SMD=-0.73,95%CI(-0.88,-0.59),P<0.01], 提升心理灵活性[MD=-2.17,95%CI (-2.77,-1.57),P<0.01]及生活质量[MD=5.27,95%CI(3.57,6.98),P<0.01]方面差异具有统计学意义。结论 ACT有助于缓解癌症患者的焦虑及抑郁情绪, 提升心理灵活性及生活质量, 对促进癌症患者的心理健康和生活质量具有积极作用。
中图分类号:
龚财芳, 赵俊宇, 游川. 接纳与承诺疗法对癌症患者心理健康和生活质量影响的meta分析[J]. 临床荟萃, 2024, 39(2): 101-107.
Gong Caifang, Zhao Junyu, You Chuan. Effect of acceptance and commitment therapy on mental health and quality of life in cancer patients: A meta-analysis[J]. Clinical Focus, 2024, 39(2): 101-107.
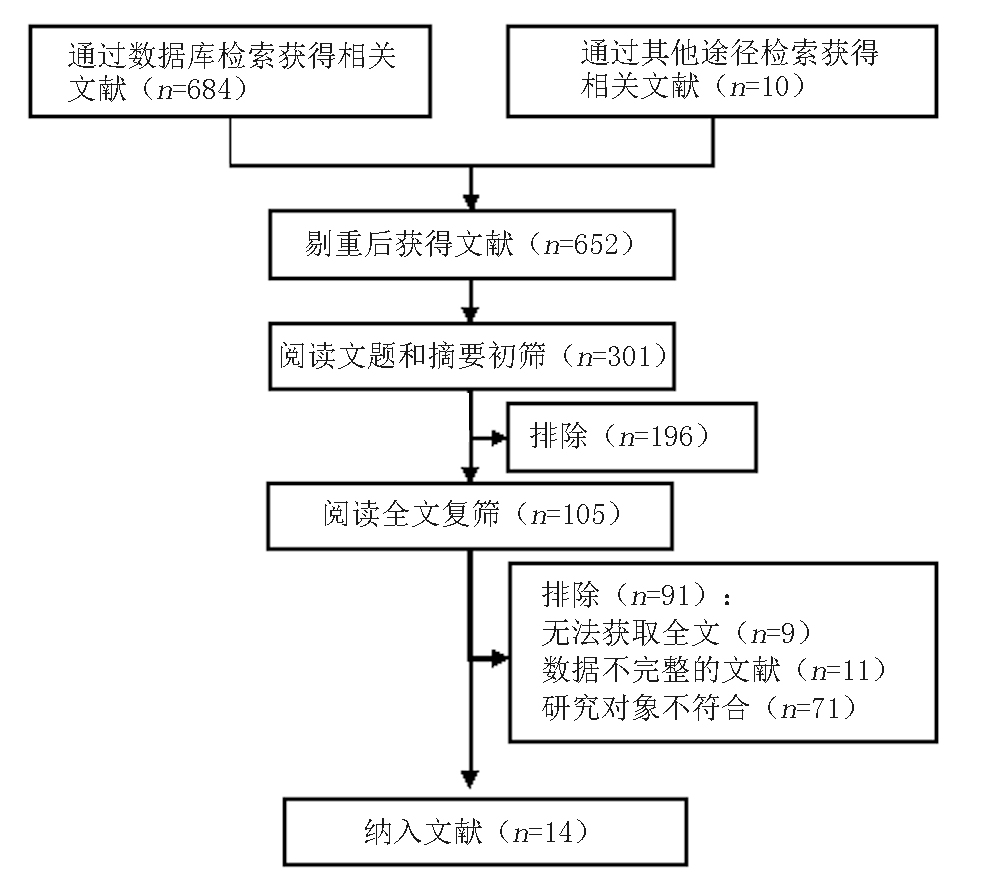
图1 文献筛选流程图 注:所检索的数据库及检出文献数具体如下:CBM(n=92)、WanFang Data(n=121)、CNKI(n=84)、VIP(n=68)、PubMed(n=132)、The Cochrane Library(n=93)、Web of Science(n=61)、Embase(n=43)
Fig. 1 Flow chart of literature screening
| 纳入文献 | 年份 (年) | 癌症 类型 | 样本量(例) | 干预措施 | 干预时间及方式 | 结局指标 | 测量工具 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 观察组 | 对照组 | 观察组 | 对照组 | ||||||||
| Shari等[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 12周,1次/3周,1 h/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Serfaty等[ | 2018 | 各种类型 | 20 | 22 | ACT+TC | TC | 3月,8次/周,1 h/次,面对面 | ③④ | HADS、FACT | ||
| Fernández-Rodríguez等[ | 2020 | 各种类型 | 12 | 17 | ACT | 常规护理 | 3月,12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| González-Fernández等[ | 2018 | 乳腺癌 | 12 | 23 | ACT | 常规护理 | 12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Johns等[ | 2019 | 乳腺癌 | 31 | 31 | ACT | SE | 6周, 1次/7d, 2 h/次,面对面 | ①② | GAD、PHQ | ||
| Li等[ | 2022 | 肺癌 | 20 | 20 | ACT | 常规护理 | 1次/周,60~90 min/次,面对面+网络视频 | ①②④ | GAD、PHQ | ||
| Mohabbat-Bahar等[ | 2015 | 乳腺癌 | 15 | 15 | ACT | 常规护理 | 4周,2次/周,90 min/次,面对面 | ①② | BAI、BHI | ||
| 周小帅[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 2周,1次/2d,30 min/次,面对面 | ①② | SAS、SDS | ||
| 姚晚侠等[ | 2020 | 乳腺癌 | 140 | 140 | ACT | 常规护理 | 3月,1次/月,面对面+电话+微信 | ①② | SAS、SDS | ||
| 潘虹等[ | 2020 | 胰腺癌 | 37 | 42 | ACT | 常规护理 | 8周,6次/周,90 min/次,面对面 | ①②③ | DASS、AAQ-Ⅱ | ||
| 王婷婷等[ | 2022 | 食管癌 | 50 | 50 | ACT | 常规护理 | 4周,面对面 | ①②③④ | SAS、SDS、AAQ-Ⅱ、QLQ-C30 | ||
| 胡迎冬等[ | 2016 | 乳腺癌 | 41 | 39 | ACT | 常规护理 | 2周,1次/2d,30~40 min/次,面对面 | ①②④ | SAS、SDS、FACT | ||
| 许湘华等[ | 2019 | 喉癌 | 24 | 24 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ③④ | AAQ-Ⅱ、FACT | ||
| 魏慧等[ | 2020 | 直肠癌 | 59 | 59 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ①② | HADS、AAQ-Ⅱ | ||
表1 纳入文献基本特征
Tab.1 Basic information of included studies
| 纳入文献 | 年份 (年) | 癌症 类型 | 样本量(例) | 干预措施 | 干预时间及方式 | 结局指标 | 测量工具 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 观察组 | 对照组 | 观察组 | 对照组 | ||||||||
| Shari等[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 12周,1次/3周,1 h/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Serfaty等[ | 2018 | 各种类型 | 20 | 22 | ACT+TC | TC | 3月,8次/周,1 h/次,面对面 | ③④ | HADS、FACT | ||
| Fernández-Rodríguez等[ | 2020 | 各种类型 | 12 | 17 | ACT | 常规护理 | 3月,12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| González-Fernández等[ | 2018 | 乳腺癌 | 12 | 23 | ACT | 常规护理 | 12次/周,90 min/次,面对面 | ①②③ | HADS、AAQ-Ⅱ | ||
| Johns等[ | 2019 | 乳腺癌 | 31 | 31 | ACT | SE | 6周, 1次/7d, 2 h/次,面对面 | ①② | GAD、PHQ | ||
| Li等[ | 2022 | 肺癌 | 20 | 20 | ACT | 常规护理 | 1次/周,60~90 min/次,面对面+网络视频 | ①②④ | GAD、PHQ | ||
| Mohabbat-Bahar等[ | 2015 | 乳腺癌 | 15 | 15 | ACT | 常规护理 | 4周,2次/周,90 min/次,面对面 | ①② | BAI、BHI | ||
| 周小帅[ | 2020 | 乳腺癌 | 30 | 30 | ACT | 常规护理 | 2周,1次/2d,30 min/次,面对面 | ①② | SAS、SDS | ||
| 姚晚侠等[ | 2020 | 乳腺癌 | 140 | 140 | ACT | 常规护理 | 3月,1次/月,面对面+电话+微信 | ①② | SAS、SDS | ||
| 潘虹等[ | 2020 | 胰腺癌 | 37 | 42 | ACT | 常规护理 | 8周,6次/周,90 min/次,面对面 | ①②③ | DASS、AAQ-Ⅱ | ||
| 王婷婷等[ | 2022 | 食管癌 | 50 | 50 | ACT | 常规护理 | 4周,面对面 | ①②③④ | SAS、SDS、AAQ-Ⅱ、QLQ-C30 | ||
| 胡迎冬等[ | 2016 | 乳腺癌 | 41 | 39 | ACT | 常规护理 | 2周,1次/2d,30~40 min/次,面对面 | ①②④ | SAS、SDS、FACT | ||
| 许湘华等[ | 2019 | 喉癌 | 24 | 24 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ③④ | AAQ-Ⅱ、FACT | ||
| 魏慧等[ | 2020 | 直肠癌 | 59 | 59 | ACT | 常规护理 | 术前1 d-术后5 d,面对面 | ①② | HADS、AAQ-Ⅱ | ||
| 结局指标 | 纳入研究 | 异质性 | 效应模型 | Meta分析结果 | ||||
|---|---|---|---|---|---|---|---|---|
| P值 | I2(%) | SMD/MD | 95%CI | Z值 | P值 | |||
| 焦虑评分 | 11 | 0.36 | 9 | 固定 | -0.99* | [-1.14,-0.85] | 13.62 | <0.01 |
| 抑郁评分 | 10 | 0.29 | 16 | 固定 | -0.68* | [-0.83,-0.54] | 9.42 | <0.01 |
| 心理灵活性 | 6 | 0.95 | 0 | 固定 | -2.17# | [-2.77,-1.57] | 7.11 | <0.01 |
| 生活质量 | 4 | 0.10 | 49 | 固定 | 0.70* | [0.43,0.97] | 5.10 | <0.01 |
表2 敏感性分析结果
Tab.2 Result of sensitivity analysis
| 结局指标 | 纳入研究 | 异质性 | 效应模型 | Meta分析结果 | ||||
|---|---|---|---|---|---|---|---|---|
| P值 | I2(%) | SMD/MD | 95%CI | Z值 | P值 | |||
| 焦虑评分 | 11 | 0.36 | 9 | 固定 | -0.99* | [-1.14,-0.85] | 13.62 | <0.01 |
| 抑郁评分 | 10 | 0.29 | 16 | 固定 | -0.68* | [-0.83,-0.54] | 9.42 | <0.01 |
| 心理灵活性 | 6 | 0.95 | 0 | 固定 | -2.17# | [-2.77,-1.57] | 7.11 | <0.01 |
| 生活质量 | 4 | 0.10 | 49 | 固定 | 0.70* | [0.43,0.97] | 5.10 | <0.01 |
| [1] |
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71 (3): 209-249.
doi: 10.3322/caac.v71.3 URL |
| [2] | 王思颖, 郑幸玲, 覃文新. 癌症患者能否长期生存?[J]. 上海交通大学学报, 2021, 55(z1):49-50. |
| [3] | 贾莉莉, 朱康宁, 张国增, 等. 癌症患者疾病感知的研究进展[J]. 中华护理教育, 2020, 17 (8):765-768. |
| [4] |
Huda N, Shaw MK, Chang HJ. Psychological distress among patients with advanced cancer: A conceptual analysis[J]. Cancer Nurs, 2022, 45 (2):E487-E503.
doi: 10.1097/NCC.0000000000000940 URL |
| [5] |
Burhan HŞ, Karadere E. Effectiveness of acceptance and commitment therapy for patients with psychosis being monitored at a community mental health center: A six-month follow-up study[J]. Alpha Psychiatry, 2021, 22 (4): 206-211.
doi: 10.5455/apd.93130 pmid: 36424936 |
| [6] |
Esmali A, Alizadeh M. The effectiveness of group psychotherapy based on acceptance and commitment on increasing of mental health and the quality of women’s life with breast cancer[J]. Biosci Biotechnol Res Asia, 2015, 12 (3): 2253-2260.
doi: 10.13005/bbra/ URL |
| [7] |
Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: Model, processes and outcomes[J]. Behav Res Ther, 2006, 44 (1): 1-25.
doi: 10.1016/j.brat.2005.06.006 pmid: 16300724 |
| [8] | Yıldız E. The effects of acceptance and commitment therapy in psychosis treatment: A systematic review of randomized controlled trials[J]. Perspect Psychiatr C, 2019, 56 (1):149-167. |
| [9] |
Sakamoto R, Ohtake Y, Kataoka Y, et al. Efficacy of acceptance and commitment therapy for people with type 2 diabetes: Systematic review and meta-analysis[J]. J Diabetes Invest, 2021, 13 (2): 262-270.
doi: 10.1111/jdi.13658 pmid: 34486816 |
| [10] |
Ghorbani V, Zanjani Z, Omidi A, et al. Efficacy of acceptance and commitment therapy (ACT) on depression, pain acceptance, and psychological flexibility in married women with breast cancer: A pre- and post-test clinical trial[J]. Trends Psychiatry Psychother, 2021, 43(2):126-133.
doi: 10.47626/2237-6089-2020-0022 pmid: 34392667 |
| [11] |
Shari NI, Zainal NZ, Ng CG. Effects of brief acceptance and commitment therapy (ACT) on subjective cognitive impairment in breast cancer patients undergoing chemotherapy[J]. J Psychosoc Oncol, 2020, 39 (6):695-714.
doi: 10.1080/07347332.2020.1856283 URL |
| [12] |
Serfaty M, Armstrong M, Vickerstaff V, et al. Acceptance and commitment therapy for adults with advanced cancer (CanACT): A feasibility randomised controlled trial[J]. Psycho Oncology, 2018, 28 (3):488-496.
doi: 10.1002/pon.v28.3 URL |
| [13] | Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version5.1.0[M]. London: The Cochrane Collaboration, 2011:150-151. |
| [14] |
Fernández-Rodríguez C, González-Fernández S, Coto-lesmes R, et al. Behavioral activation and acceptance and commitment therapy in the treatment of anxiety and depression in cancer survivors: A randomized clinical trial[J]. Behav Modif, 2020, 45 (5):822-859.
doi: 10.1177/0145445520916441 URL |
| [15] |
González-Fernández S, Fernández-Rodríguez C, Paz-Caballero M, et al. Treating anxiety and depression of cancer survivors: Behavioral activation versus acceptance and commitment therapy[J]. Psicothema, 2018, 30 (1):14-20.
doi: 10.7334/psicothema2017.396 pmid: 29363465 |
| [16] | Johns SA, Stutz PV, Talib TL, et al. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: A 3-arm pilot randomized controlled trial[J]. Cancer Am Cancer Soc, 2019, 126 (1):211-218. |
| [17] | Li H, Jin X, Ng M, et al. Effects of Acceptance and commitment therapy on fatigue interference and health-related quality of life among patients with advanced lung cancer: A pilot randomized controlled trial[J]. Asia Pac J Oncol Nur, 2022, 9 (8):100102. |
| [18] | Mohabbat-Bahar S, Maleki-Rizi F, Akbari ME, et al. Effectiveness of group training based on acceptance and commitment therapy on anxiety and depression of women with breast cancer[J]. Iran J Cancer Prev, 2015, 8 (2):71-6. |
| [19] | 周小帅. 接纳与承诺疗法在乳腺癌根治术后患者护理中的应用效果[J]. 中国民康医学, 2020, 32(11):151-153. |
| [20] | 姚晚侠, 何苗, 李春华, 等. 接纳与承诺疗法在乳腺癌术后化疗患者中的应用及效果观察[J]. 护士进修杂志, 2020, 35(24):2275-2277. |
| [21] | 潘虹, 罗冰, 遆甜, 等. 接受与承诺疗法对晚期胰腺癌病人心理应激的影响[J]. 护理研究, 2020, 34(7):1279-1282. |
| [22] |
王婷婷, 杨孝苹. 接纳与承诺疗法对食管癌术后患者负性情绪及生活质量的影响[J]. 中国临床护理, 2022, 14(2):90-93.
doi: 10.3969/j.issn.1674-3768.2022.02.006 |
| [23] | 胡迎冬, 蒋维连. 接纳与承诺疗法对乳腺癌术后患者焦虑抑郁情绪及生命质量的影响[J]. 中国实用护理杂志, 2016, 32(29):2265-2268. |
| [24] | 许湘华, 欧美军, 谢婵娟, 等. 接纳与承诺疗法在喉癌术后患者中的应用效果[J]. 解放军护理杂志, 2019, 36(5):6-10. |
| [25] | 魏慧, 薛晓红, 刘梅红. 接纳与承诺疗法对直肠癌患者疼痛及负性情绪的影响[J]. 癌症进展, 2020, 18(23):2472-2475. |
| [26] |
Chinh K, Mosher CE, Brown LF, et al. Psychological processes and symptom outcomes in mindfulness-based stress reduction for cancer survivors: A pilot study[J]. Mindfulness, 2020, 11 (4): 905-916.
doi: 10.1007/s12671-019-01299-0 pmid: 33456623 |
| [27] | 陶元玲, 孙丽, 张立力. 晚期癌症患者灵性应对现状及影响因素研究[J]. 护理管理杂志, 2022, 22(2):105-110. |
| [28] |
Mitchell AJ, Ferguson DW, Gill J, et al. Depression and anxiety in long- term cancer survivors compared with spouses and healthy controls: A systematic review and meta-analysis[J]. Lancet Oncol, 2013, 14 (8):721-32.
doi: 10.1016/S1470-2045(13)70244-4 pmid: 23759376 |
| [29] |
Walker J, Magill N, Mulick A, et al. Different independent associations of depression and anxiety with survival in patients with cancer[J]. J Psychosom Res, 2020, 138 110218.
doi: 10.1016/j.jpsychores.2020.110218 URL |
| [30] | Wersebe H, Lieb R, Meyer AH, et al. The link between stress, well-being, and psychological flexibility during an acceptance and commitment therapy self-help intervention[J]. Int J Clin Hlth Psyc, 2017, 18 (1):60-68. |
| [31] |
Lv J, Zhu L, Wu X, et al. Study on the correlation between postoperative mental flexibility, negative emotions, and quality of life in patients with thyroid cancer[J]. Gland Surg, 2021, 10 (8):2471-2476.
doi: 10.21037/gs-21-424 pmid: 34527559 |
| [32] |
Li H, Wu J, Ni Q, et al. Systematic review and meta-analysis of effectiveness of acceptance and commitment therapy in patients with breast cancer[J]. Nurs Res, 2021, 70 (4):E152-E160.
doi: 10.1097/NNR.0000000000000499 pmid: 33492055 |
| [33] |
Twohig MP, Levin ME. Acceptance and commitment therapy as a treatment for anxiety and depression: A review[J]. Psychiat Clin N Am, 2017, 40 (4):751-770.
doi: 10.1016/j.psc.2017.08.009 URL |
| [34] |
Yu L, Mccracken LM. Model and processes of acceptance and commitment therapy (ACT) for chronic pain including a closer look at the self[J]. Curr Pain Headache R, 2016, 20(2):12.
doi: 10.1007/s11916-016-0541-4 pmid: 26803836 |
| [35] |
Coto-Lesmes R, Fernández-Rodríguez C, González-Fernández S. Acceptance and commitment therapy in group format for anxiety and depression: A systematic review[J]. J Affect Disorders, 2019, 263: 107-120.
doi: 10.1016/j.jad.2019.11.154 URL |
| [36] |
Bai Z, Luo S, Zhang L, et al. Acceptance and commitment therapy (ACT) to reduce depression: A systematic review and meta-analysis[J]. J Affect Disorders, 2019, 260:728-737.
doi: 10.1016/j.jad.2019.09.040 URL |
| [37] |
Zhao C, Lai L, Zhang L, et al. The effects of acceptance and commitment therapy on the psychological and physical outcomes among cancer patients: A meta-analysis with trial sequential analysis[J]. J Psychosom Res, 2020, 140 110304.
doi: 10.1016/j.jpsychores.2020.110304 URL |
| [1] | 苏芮, 王存凯, 王鼎鑫, 蔡聪会, 张建, 侯洪涛, 白云. 肝硬化患者抗凝治疗有效性和安全性的meta分析[J]. 临床荟萃, 2025, 40(4): 293-303. |
| [2] | 王英, 钟博华, 王丽芳, 朗秋燕, 罗海彬, 王书林, 李春朋, 廖敏. 儿科体外膜肺氧合支持患者院内感染流行病学特征的meta分析[J]. 临床荟萃, 2025, 40(1): 14-20. |
| [3] | 王琳, 王婷, 蒲晓岚, 鞠梅. 老年人口腔健康状况与认知功能纵向队列研究的meta分析[J]. 临床荟萃, 2024, 39(8): 677-683. |
| [4] | 叶智博, 李可勇, 阙昌浩, 王亚平, 苟云久. 腹腔镜Heller肌切开术与经口内镜下肌切开术治疗贲门失弛缓症疗效及安全性的meta分析[J]. 临床荟萃, 2024, 39(8): 684-692. |
| [5] | 岳江红, 王恒, 蔡钢, 张选明, 彭曦. 索格列净治疗2型糖尿病疗效和安全性的meta分析[J]. 临床荟萃, 2024, 39(7): 581-592. |
| [6] | 王彩贞, 苗丽娜, 陈源, 李双成. 高频迷走神经刺激治疗难治性癫痫有效性的meta分析[J]. 临床荟萃, 2024, 39(7): 593-597. |
| [7] | 高铭, 刘昊, 于航, 林霖, 张紫杰, 熊颖. 超声造影对局灶性睾丸病变诊断价值的meta分析[J]. 临床荟萃, 2024, 39(5): 389-395. |
| [8] | 员笑笑, 李淑芬, 孙芳. 免疫功能正常成人腺病毒肺炎患者临床特征的meta分析[J]. 临床荟萃, 2024, 39(4): 293-303. |
| [9] | 孙帅刚, 翟亚玲, 张文惠, 田慧娟. 扁桃体切除术治疗IgA肾病的疗效评价:一项meta分析[J]. 临床荟萃, 2024, 39(3): 197-207. |
| [10] | 李冠珠, 杨亚婷, 邓金和, 邵兰, 曾朝坤. 垂体后叶素联合肾上腺素应用于心肺复苏治疗效果的meta分析[J]. 临床荟萃, 2024, 39(3): 208-215. |
| [11] | 张琦, 孙增鑫, 赵越, 袁野, 秦小露, 吕红香, 尹昱, 张雅文. 经颅直流电刺激对脑卒中患者单侧忽略康复效果的影响: 网状meta分析[J]. 临床荟萃, 2024, 39(12): 1061-1072. |
| [12] | 张雪梅, 张先, 董雪, 郭燕杰. 认知行为疗法对自杀倾向患者心理状态的meta分析[J]. 临床荟萃, 2024, 39(12): 1073-1080. |
| [13] | 贺田, 韩琳秋, 施祖新, 沈鸣雁. 肝移植患者术后多重耐药菌感染发生率及危险因素的meta分析[J]. 临床荟萃, 2024, 39(11): 965-973. |
| [14] | 赵家华, 马庆华, 于江华. 维生素D缺乏与老年人群直立性低血压:系统综述与meta分析[J]. 临床荟萃, 2024, 39(10): 869-876. |
| [15] | 冯雨慧, 邹兰兰, 李凡, 崔晨航, 乔俊英. 血清血管性血友病因子在急性肺损伤/急性呼吸窘迫综合征患者中表达的meta分析[J]. 临床荟萃, 2024, 39(10): 877-881. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||